Anaemia and prolonged length of stay: a retrospective analysis of a 1-year cohort of inpatients.
M. Colafelice,1 R. Mastrosanti,2 M. Ciabattini,2 M. Maurici,2 F. Lauria,1 L. Morciano,2 F. Lucaroni2
1 Sant’Eugenio Hospital
2 University of Rome Tor Vergata
Introduction
Anaemia is a widespread disease, globally affecting almost 2 billion individuals and therefore being considered an important health burden.1 Mild, moderate and severe anaemia together determine over 60 million years of life lived with disability (YLDs) all over the world. Only in Italy, it has been estimated that anaemia affects nearly 20% of the entire population,2 with prevalence rate rapidly increasing by age, exceeding 40% in individuals who are older than 80 years, in particular among the hospitalised patients.3 According to international studies, 58.4% to 74% of inpatients, including those with normal Hb levels at the hospital admission, have anaemia.4-6 Besides being a common disorder, not only in older people, anaemia can rapidly develop to multiple co-morbidities and to the impairment of self-sufficiency.7,8
Moreover, it is often an under-reported disease, both in outpatients and inpatients, because it is rarely considered as a main pathological entity. Therefore, except in the cases of acute blood loss, it may remain untreated.9
Anaemia is then associated with the increase in healthcare services utilisation and with the worsening of different health outcomes, irrespective of the reasons of hospital admission: it contributes to delay hospital discharge and to increase mortality and morbidity rates,4-6,9 thus leading to the rise of the economic burden of disease, due both to direct and indirect costs of anaemia.10
In recent years, there is a growing awareness of a pathogenetic association between frailty and anaemia in the elderly, and current scientific evidence highlights the role of anaemia as an early biomarker of frailty condition.9,11,12
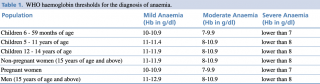
Anaemia is defined by low amount of red blood cells (RBCs) or insufficient haemoglobin (Hb) levels for physiological needs. According to WHO,13 the Hb threshold values to diagnose anaemia are 13 g/dL for men and 12 g/dL for non-pregnant women, with age difference and severity stratification, as shown in Table 1.
Anaemia and prolonged length of stay a retrospective analysis of a 1-year cohort of inpatients.
The most frequent cause of anaemia is nutrient deficiency, in particular iron deficiency, though many conditions, going from chronic diseases to infections, may contribute to determine it.14,15
Anaemia is often a predictable and relatively simply treatable disorder, by administration of micronutrients,9,16-19 and its prevalence could be significantly reduced by the introduction of specific diagnostic and treatment pathways, in a multi-dimensional approach, involving also General Practitioners and Local Health Units.9
The aim of the study is to examine anaemia profiles as independent predictors of increased length of hospital stay (LOS) and in-hospital mortality through the analysis of administrative data in an Italian Hospital and to compare anaemia with other common chronic pathologic conditions which are known to be associated with a LOS increase, including dementia,20 respiratory impairments,21 diabetes22 and chronic kidney failure.23
Material and Methods
A monocentric observational retrospective study was performed in 2016 in Sant’ Eugenio Hospital, a public hospital in Rome with nearly 570 ordinary beds. All the discharge from 01/01/2016 to 12/31/2016 were evaluated, irrespective from main diagnosis, age or gender. Only ordinary admissions of patients aged over 14 were taken into consideration for the analysis.
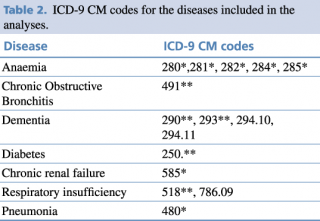
Chronic diseases investigated as predictive factors for high LOS and increased in-hospital mortality are listed in Table 2, with their specific ICD-9 CM codes. Diagnoses were defined according to primary and secondary diagnoses at discharge. In case of re-hospitalisations during the evaluated period, only the first access was considered.
Besides those shown in Table 2, also gender and educational level were included in the analysis as independent variables.
Primary outcome measures investigated were in-hospital mortality and prolonged length of stay, defined as mean LOS + 1 SD.
Table 2. ICD-9 CM codes for the diseases included in the analyses.
Statistical analysis
The impact of chronic diseases on hospital stay (LOS) and in-hospital mortality was evaluated by multivariate binary logistic regression, using the IBM SPSS statistical software (Illinois, Chicago, v.24).
Furthermore, Mantel-Haenszel adjustment by age was achieved for LOS, since the significant age difference between the two study arms, carried out by ANOVA test.
A p value of 0.05 was identified as threshold to reject the null hypothesis.
Results
In 2016, 11,579 ordinary hospital admissions were recorded in Sant’ Eugenio Hospital in Rome. Population sample was constituted by 55.9% (N=6,475) of women and 44.1% (N=5,104) of men, with a mean age of 62.6 (SD ±20.3) years and a median of 67 (IQ 46-79). Furthermore, the most part of them (57.5%, N=6,655) had high educational level (High School Diploma or above).
An overall number of 1,065 (9.2%) hospital stays showed anaemia, according to discharge records. The most part of codified cases were chronic anaemias (42.1%, N=448), followed by 21.8% (N=232) deficiency anaemias, and 2.1 % (N=22) thalassemia. One case by three (N=363) was recorded as “other types of anaemias” (data not shown).
Inpatients had an average LOS of 8.26 (SD ±9.63) days, therefore prolonged LOS corresponded to an hospital stay equal or over 18 days. Those with high LOS, accounting to nearly 10% of the population sample, were older: they had a mean age of 68.9 (SD ±17.4) years compared with 61.9 (SD ±20.5) of patients with lower LOS (p value 0.000, by ANOVA test) (data not shown).
Nearly 1 patient out of 2 (48.5%) was discharged home, whereas assisted discharge accounted for 32.9%, transfers to other institutes for 9.4% and 5.8% of admissions resulted in in-hospital deaths.
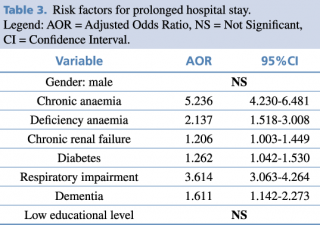
Prolonged LOS was statistically significant associated with a number of comorbidities. Chronic anaemia, respiratory impairment and deficiency anaemia showed the strongest association, with adjusted Odds Ratios (AORs) of 5.236 [95%CI 4.230-6.481], 3.614 [95%CI 3.063-4.264] and 2.137 [95%CI 1.518-3.008], respectively (Table 3). Conversely, no significant association with gender and educational level emerged.
Table 3. Risk factors for prolonged hospital stay.
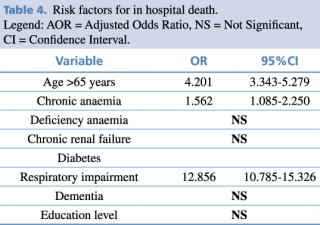
Concerning the impact of comorbidities on in-hospital death, the role of chronic anaemia decreased in magnitude [OR 1.562; 95%CI 1.085-2.250], whereas the impact of respiratory impairment became four times higher [OR 12.856; 95%CI 10.785-15.326]. All the other assessed anaemia profiles showed no statistically significant association with mortality (see Table 4). Not surprisingly, the risk of death during hospital stay increased among elderly people.
Table 4. Risk factors for in hospital death.
Discussion
Strenghts and limitations
By the best of our knowledge, this is one of the few studies comprehensively assessing anaemia profiles as independent risk factors for both LOS and in-hospital mortality in Italy. However, the study presents some limitations. Anaemia was only defined according to discharge records, although some recent evidence shows the high underestimate of anaemia cases exclusively based on administrative data.9 Comparing Hb levels both at admission and discharge would be more useful to define the magnitude of anaemia prevalence, eventually achieving also stratification by severity (i.e. mild, moderate or severe anaemia).9
Chronic diseases were defined by the evaluation of primary diagnosis and one of the five secondary diagnoses, thus not considering all the diagnostic codes included in discharge records. Since chronic diseases, anaemia in particular, are very seldom included within primary and first secondary diagnoses, because of their low impact in acute resource consumption during hospital stay, the study might be affected by underestimation of the disease burden of investigated chronic diseases. This limitation might explain the low overall prevalence of anaemia (9.2%), compared with international data, ranging between 58.4% to 74%.4-6
Synthesis of the results
Among the chronic diseases with highest prevalence, anaemia behave as the strongest independent risk factor, both for long in-hospital stay and for in-hospital mortality. Respiratory impairment only impacted more than anaemia on inpatients mortality. Deficiency anaemia, the profile accounting the most part of anaemia diagnoses at discharge, is an independent risk factor only for prolonged in-hospital stay, whereas no statistically significant association was found with in-hospital mortality. Conversely, anaemia due to chronic disorders showed a relevant impact on both outcomes.
Our results on mortality are consistent with other international data. In two elderly cohorts, anaemia was found to be significantly associated with a relative risk of death of 1.61, [95% CI 1.34-1.93]24 and a mortality risk of 1.60 [95% CI 1.24-2.06].25
Chronic anaemia increased more than 5 times the risk of having a hospital stay longer than 18 days, irrespectively from age and gender. These results show the same direction of scientific evidence, although they don’t have the same magnitude: recent studies showed an increased risk of prolonged LOS ranging from 1.37 [95%CI 1.01- 1.79] for all anaemias4 to 2.18 [95%CI 2.11-2.26] for moderate/severe anaemias,26 with a median LOS increase of 1.5 days by unit of Hb decrease.27
The difference in magnitude is partially explainable by the choice of the Authors to evaluate the different profiles of anaemia as independent risk factors for negative in-hospital outcomes. Furthermore, in the advanced age groups, where anaemia has the highest prevalence, a relationship with a more complex condition, frailty, should be considered, as recent studies suggest.12 Indeed, frailty and chronic anaemia share a common pathogenic path, characterised by chronic inflammation, induced by immuno-senescence associated changes and oxidative stress.12 Deficiency anaemia also might be indirectly affected by the interaction with frailty and chronic anaemia. Indeed, these two anaemia profiles are physio-pathologically associated entities: frail subjects with chronic anaemia show an increase in hepcidin, a peptide inhibiting the release of iron from depots, inducing functional iron deficiency.12
Since the complexity of the pathogenetic interaction, it could be promising to investigate anaemia, by Hb levels evaluation, together with a number of possible proxy of frailty, such as blood albumin, creatinine, BUN, GOT and GPT, in order to build a frailty predictive index or to integrate Frailty Risk Index12,28 with laboratory parameters routinely measured.
Conclusions
There is plenty of studies available showing the negative impact of anaemia on different health outcomes, but few considering anaemia profiles as independent risk factors. In this study we observed how the magnitude of the association with negative inpatients health outcomes substantially increases when specific anaemia profiles are considered as independent factors. This is true in particular for anaemia induced by chronic disease, probably for the complexity of the disorders included in this classification, and to a lesser extent for deficiency anaemia. Since the availability of effective therapies, in particular for deficiency disorders, early identification of people at risk, through an active “case finding” in the hospital using risk prediction tools, might be considered nowadays a main strategy to reduce in-hospital mortality and prolonged hospital length of stay. Furthermore, hospitals are not the proper settings for treatment of such complex disorders. Patients-targeted therapeutic paths should be built at the outpatient care level, in order to manage patients with a multi-dimensional approach, involving General Practitioners, family nurses, nutritionists and other healthcare professionals.
References
- Staibano P, Perelman I, Lombardi J, Davis A, Tinmouth A, Carrier M, Stevenson C, Saidenberg E. Patient-Centered Outcomes in the Management of Anaemia: A Scoping Review. Transfus Med Rev. 2018 Jul 12. pii: S0887-7963(18)30051-8.
- Kassebaum NJ; GBD 2013 Anaemia Collaborators. The Global Burden of Anaemia. Hematol Oncol Clin North Am. 2016 Apr; 30(2):247-308
- Berliner N. Anaemia in the Elderly. Trans Am Clin Climatol Assoc. 2013; 124:230-7. PubMed PMID: 23874029; PubMed Central PMCID: PMC3715932.
- Zaninetti C, Klersy C, Scavariello C, Bastia R, Balduini CL, Invernizzi R. Prevalence of Anaemia in Hospitalized Internal Medicine Patients: Correlations with Comorbidities and Length of Hospital Stay. Eur J Intern Med. 2018 May; 51:11-17.
- Koch CG, Li L, Sun Z, et al. Hospital-Acquired Anaemia: Prevalence, Outcomes, and Healthcare Implications. J Hosp Med 2013; 8: 506-12
- Goodnough LT, Maniatis A, Earnshaw P, et al. Detection, Evaluation, and Management of Preoperative Anaemia in the Elective Orthopaedic Surgical Patient: NATA Guidelines. Br J Anaesth 2011; 106: 13-22
- Stauder R, Valent P, Theurl I. Anemia at Older Age: Etiologies, Clinical Implications, and Management. Blood. 2018 Feb 1; 131(5):505-514.
- Chaves PH1, Ashar B, Guralnik JM, Fried LP - Looking at the Relationship Between Haemoglobin Concentration and Prevalent Mobility Difficulty in Older Women. Should the Criteria Currently Used to Define Anaemia in Older People Be Re-evaluated? J Am Geriatr Soc. 2002 Jul; 50(7):1257-64.
- Articolo su Anemia PTV.
- Smith RE Jr. The Clinical and Economic Burden of Anaemia. Am J Manag Care. 2010 Mar; 16 Suppl Issues: S59-66. Review. PubMed PMID: 20297873
- Legramante JM, Morciano L, Lucaroni F, Gilardi F, Caredda E, Pesaresi A, Coscia M, Orlando S, Brandi A, Giovagnoli G, Di Lecce VN, Visconti G, Palombi L. Frequent Use of Emergency Departments by the Elderly Population When Continuing Care Is Not Well Established. PLoS One. 2016 Dec 14; 11(12): e0165939.
- Röhrig G. Anemia in the Frail, Elderly Patient. Clin Interv Aging. 2016 Mar 17; 11:319-26.
- WHO. Haemoglobin Concentrations for the Diagnosis of Anaemia and Assessment of Severity. Geneva (Switzerland): World Health Organization; 2011.
- De Franceschi L, Iolascon A, Taher A, Cappellini MD. Clinical Management of Iron Deficiency Anaemia in Adults: Systemic Review on Advances in Diagnosis and Treatment. Eur J Intern Med. 2017 Jul; 42:16-23.
- Camaschella C. Iron-Deficiency Anaemia. N Engl J Med. 2015 May 7; 372(19):1832-43.
- Anand IS. Anaemia and Chronic Heart Failure Implications and Treatment Options. J Am Coll Cardiol. 2008; 52:501–511
- Robinson B, Artz AS, Culleton B, et al. Prevalence of Anaemia in the Nursing Home: Contribution of Chronic Kidney Disease. J Am Geriatr Soc 2007; 55:1566 – 1570.
- Lindenfeld J. Prevalence of Anaemia and Effects on Mortality in Patients with Heart Failure. Am Heart J. 2005; 149:391–401.
- Beghe C, Wilson A, Ershler WB. Prevalence and Outcomes of Anaemia in Geriatrics: A Systematic Review of Literature. Am J Med 2004; 116: 3S–10S.
- Möllers T, Stocker H, Wei W, Perna L, Brenner H. Length of Hospital Stay and Dementia: A Systematic Review of Observational Studies. Int J Geriatr Psychiatry. 2019 Jan; 34(1):8
- Alshabanat A, Otterstatter MC, Sin DD, Road J, Rempel C, Burns J, van Eeden SF, FitzGerald JM. Impact of a COPD Comprehensive Case Management Program on Hospital Length of Stay and Readmission Rates. Int J Chron Obstruct Pulmon Dis. 2017 Mar 21; 12:961-971.
- Valent F, Tonutti L, Grimaldi F. Does Diabetes Mellitus Comorbidity Affect In-Hospital Mortality and Length of Stay? Analysis of Administrative Data in an Italian Academic Hospital. Acta Diabetol. 2017 Dec; 54(12):1081-1090.
- Nishikawa K, Takahashi K, Yamada R, Kinaga T, Masato M, Yamamoto M. Influence of Chronic Kidney Disease on Hospitalization, Chronic Dialysis, and Mortality in Japanese Men: A Longitudinal Analysis. Clin Exp Nephrol. 2017 Apr; 21(2):316-323.
- Penninx BW, Pahor M, Woodman RC, Guralnik JM. Anemia in Old Age Is Associated with Increased Mortality and Hospitalization. J Gerontol A Biol Sci Med Sci. 2006 May; 61(5):474-9. PubMed PMID: 16720744.
- Izaks GJ, Westendorp RG, Knook DL. The Definition of Anemia in Older Persons. JAMA. 1999 May 12; 281(18):1714-7. PubMed PMID: 10328071.
- Krishnasivam D, Trentino KM, Burrows S, Farmer SL, Picardo S, Leahy MF, Halder A, Chamberlain J, Swain S, Muthucumarana K, Waterer G. Anaemia in Hospitalized Patients: An Overlooked Risk in Medical Care. Transfusion. 2018 Nov; 58(11):2522-2528.
- Lin RJ, Evans AT, Chused AE, Unterbrink ME. Anaemia in General Medical Inpatients Prolongs Length of Stay and Increases 30-Day Unplanned Readmission Rate. South Med J. 2013 May; 106(5):316-20.
- Ng TP, Feng L, Nyunt MS, Larbi A, Yap KB. Frailty in Older Persons: Multisystem Risk Factors and the Frailty Risk Index (FRI). J Am Med Dir Assoc. 2014 Sep; 15(9):635-42.