A new approach to assess the health of workers
Leonardo Palombi,1 Cristina Ambrosone,1 Laura Morciano,1 Ersilia Buonomo,1 Andrea Malizia,1,2 Stefania Moramarco,1 Gennaro Cerone,1 Andrea Berardi,1 Danilo De Angelis,3 Anna Aniuskevich1 and Francesca Lucaroni1
1University of Rome Tor Vergata, Dept. of Biomedicine and Prevention, Via Montpellier 1, 00133 Roma
2 International CBRNe Master Courses, Via del Politecnico 1, 00133 Roma
3 PHOENIX ESD Srl
Introduction
Occupational health represents a main issue worldwide because workers amount to half the world’s population.1 Relevant changes in occupational health – swinging from constant identification of new workplace health hazards to changing nature of work itself – are responsible of the increasing trend in occupational disease and of the consequent higher attention reserved for this issue.
Indeed, work conditions have a huge impact on health worldwide, being responsible for 2.3 million deaths by year. More than 50% of global burden of deaths is due to neoplasms (32%) and circulatory diseases (23%), followed by occupational accidents and infectious diseases.2
In Italy an overall number of 21,822 occupational diseases have been recorded in 2014,3 with a constantly increasing trend.4
For work activities that expose the workers to risk agents, the current Italian legislation establishes the limits of exposure that must not be exceeded and the health surveillance (HS) protocol that need to be followed.5
The HS consists of systematic, regular and appropriate procedures to detect early signs of work-related pathologies among workers exposed to health risks (of physical, chemical, biological or ergonomic nature) likely to cause a work-related illness after a variable period of exposure.6,7,8
Health Surveillance is a key step of occupational safety and health management: the findings from HS can be also used to quantify work related diseases at a population level, estimating incidence and prevalence rate,9 to assess the adequacy of control measures, to undertake preventive actions, and to provide health education.
The type of medical examinations to which the worker is subjected, and therefore the health protocol defined by the competent doctor (CD, medico competente), is related to the specific health risks, each worker is exposed to.
Hydrocarbons represent one of the main occupational risk factors. Inhalation, that is the main route of exposure for these chemicals, is potentially associated with arrhythmia, cancer, lung disease.10
The COVA, core system of ENI’s activities in Southern Italy, is mainly dedicated to the treatment of hydrocarbons. The centre has been in business since 2001 in the industrial area of Viggiano (PZ – Italy) and it occupies an area of approximately 180,000 square meters.
Because of the potentially high risk of COVA’s workers due to chronic exposure at hydrocarbons, this work aims to be a case study, focused on evaluating occupational health. We adopted a new approach, integrating health surveillance, as prescribed by current legislation, with elements of epidemiology – comparing, for instance, local and national prevalence rates for the main communicable and non-communicable diseases – and assessing individual risk factors (smoke, alcohol consumption, nutritional habits and physical activity).
At the best of our knowledge, this is the first time occupational surveillance measures are combined with epidemiological surveillance, yet too underutilized in workers’ health care management.11
Methods
The clinical records related to the periodical health surveillance carried out by the CD on ENI workers during the period 1999-2018 were analyzed. The following variables were evaluated: identification code, age, gender, working duties and tasks, pathologies in progress. Personal data, working duties and pathologies in progress have been codified using the ICD9 international classification, up to a maximum of three per worker, and inserted into an Excel™ file with an encrypted key. Furthermore, personal data and workers’ health conditions were anonymized by assigning specific alphanumeric code for each of the workers. Data were processed using SPSS v.23 statistical-epidemiological software, in order to describe the main characteristics of the analyzed sample and to estimate the prevalence of chronic-degenerative diseases (hypertension, tumors, rhythm disorders, etc.). Prevalence data were compared with the national data, through χ2 statistical test. The significance for all tests was set at 5% (p-values <0.05 were considered significant; p-values are associated with hypothesis testing and with defining a null and an alternative hypothesis).
The previous described evaluation was integrated with a questionnaire on lifestyles, validated by the Italian National Health Institute “Istituto Superiore di Sanità (ISS)”;12 the questionnaire has investigated educational qualification, profession, anthropometric parameters, diet and nutritional status. The nutritional status was assessed considering the Body Mass Index (BMI), physical activity and alcohol consumption, including also information on smoking and medication. This assessment was carried out on a sub-sample of the population (258 out of 853, corresponding to 30.2% of the sample), in order to ensure a correct assessment of occupational and exposure risk factors in an epidemiological framework that took into account how much the worker is exposed to the main risk factors for chronic-degenerative diseases.
Results
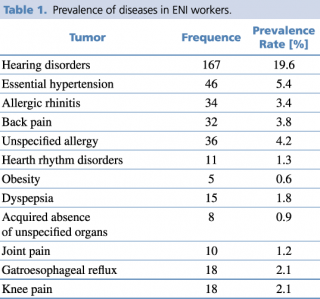
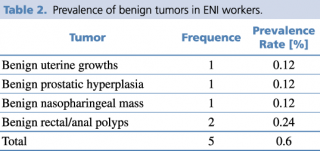
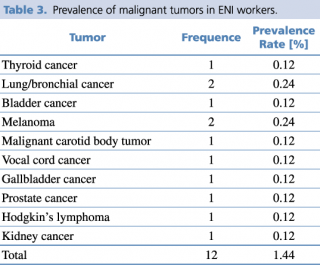
The present work was carried out analyzing the documentation relating to health surveillance collected by the CD of 853 ENI workers (6.6% females - 93.4% males), with an average age of 45.36 years (S.D. ±11.85). The workers who served at ENI in the period 1999-2018 show a prevalence rate of chronic-degenerative diseases as reported in Table 1. The most prevalent diseases are hearing disorders (19.6%), including mono or bilateral hypoacusias (transmissive or sensorineural type), and essential hypertension (5.4%). Furthermore, as presented in Tables 2 and 3, five cases of benign tumor and 12 cases of malignant tumor were detected in the investigated period, with a prevalence of 0.6% and 1.44%, respectively.
Prevalence of diseases in ENI workers
Prevalence of benign tumors in ENI workers
Prevalence of malignant tumors in ENI workers
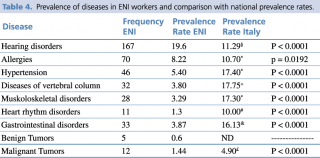
Table 4 shows the data related to the investigated pathologies compared with the data of national prevalence and the relative significance of χ2 test. Compared with the national prevalence data, a significant increase in the prevalence of hearing disorders is reported in ENI workers, while the prevalence of all the other diseases is reduced. These discrepancies could not be uniquely linked to a real difference in the prevalence of pathologies among COVA’s workers; it could instead reflect a greater attention to some diseases and an underestimation of other diseases not specifically related to professional exposure or not specifically monitored according the current legislation.
Prevalence of diseases in Eni workers and comparison with national prevalence rates
In order to investigate other risk factors, as individual behaviour (lifestyle), a subgroup of 258 ENI workers [93.8% men, average age 40.3 years (S.D. ±9.6)] have been subjected to a lifestyle questionnaire, validated by the Italian National Health Institute. The survey investigated four key lifestyle areas: nutrition, physical activity, smoking and alcohol consumption.
The workers in the evaluated sample have an average BMI of 26.4 kg/m2 (S.D. ±3.9), with a median value of 25.8 (IQ 24.2-28); this data show a condition of overweight (BMI above 25) in 62% of cases. Furthermore, a significant proportion of workers (54.3%) do not regularly practice physical activity.
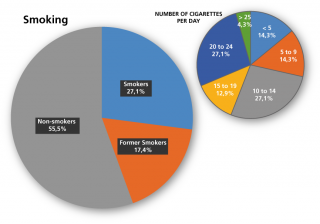
As shown in Figure 1, the 27.1% of workers are smokers, with an average consumption of 11.5 cigarettes a day. The 17.4% of the sample is composed by former smokers, who have stopped smoking on average from 10.7 years (S.D. ±11.1). It’s important to note the relationship between BMI and smoking: the 75.7% of the sample have a BMI>25, showing a condition of overweight/obesity.
Distribution of smokers non smokers and former smokers
Regarding alcohol consumption, 81% of the sub-sample of ENI workers declares to consume alcohol, a significantly higher percentage than the national one (55.1%, p-value <0.0001), with an average weekly consumption of 1.6 alcohol units (0.2 alcohol units daily) (S.D. ±1.3).
Discussion
The epidemiological surveillance approach allows identifying potential workplace hazards, recognizing high-risk groups for targeting preventive efforts and providing a mechanism for evaluating interventions. It should be valuable in supporting management decisions relating to health promotion and disease prevention programs, as well as basic clinical needs of employees.11
The study contains some limitations, mainly due to the unavailability of codified medical documentation, to the observation of the lifestyle of a reduced sub-population, to the possibility to provide only cumulative prevalence data, and to the accessibility only to national prevalence data not related to a population of working age and mainly of male gender, as ENI’s.
Albeit these intrinsic limitations, our study represents a pioneering work in the field of occupational medicine: through an integrated approach between epidemiology and community health, it allows going beyond the simple fulfillment of legislation requirements to embrace a holistic management of workers’ health.
By comparing the prevalence of the main chronic-degenerative diseases in the ENI workers with the national data, a significant increase in hearing disorders was identified. Contrariwise, a reduction of heart rhythm disorders, arterial hypertension, neoplasms, musculoskeletal disorders (low back pain, arthralgias), allergopathy, gastroesophageal reflux was recorded. The discrepancy between COVA’s workers’ prevalence of diseases compared with national data is not uniquely imputable to work conditions. The significant decrease of main chronic diseases, not even supported by the results of the questionnaire on individual lifestyles, is probably due to a pathologies under-reporting rather than directly related to occupational exposure. Indeed, the questionnaire results show that the workers of the COVA have lifestyles significantly worse compared with the national data, in particular concerning the nutritional status, alcohol consumption and sedentary lifestyle, three of the main risk factors for chronic-degenerative diseases.13 Regarding nutrition, the evaluation of the BMIs showed that the rate of overweigh/obese subjects (BMI > 25) is 62%, a strong increase if compared to 42.2% of the national data (p-value <0.0001).14 A huge difference is also observed for physical activity: sedentary workers are the 54.3% of the sample, against a national value of 32.5% (p-value <0.0001).15
Regarding alcohol consumption, 81% of the sub-sample of ENI workers declares to consume alcohol, a significantly higher percentage than the national one (55.1%, p-value <0.0001),16 with an average weekly consumption of 1.6 alcohol units (S.D. ±1.3).
Differently, no significant difference in cigarette smoke trend was recorded in comparison with national data.17
Multi-factorial origin of the majority of chronic-degenerative diseases, and the bad individual lifestyle of COVA’s workers, make the new approach proposed in this work, integrating elements of epidemiology and community health, a method of excellence for surveillance of the health status of workers and the starting point for primary, secondary and tertiary prevention interventions involving local communities.
Acknowledgments
The authors would like to thank Dr. Orlando Cenciarelli for the suggestions on the data presentation.
References
- World Health Organization (WHO) [Internet]. Workers’ Health: Global Plan of Action. (2007) [cited 2018 May 29]. Available from: http://www.who.int/occupational_health/WHO_health_assembly_en_web.pdf;
- Rushton L. The Global Burden of Occupational Disease. Curr Environ Healt Rep. (2017) Sep; 4(3):340-348;
- Istituto Nazionale di Statistica (ISTAT) [Internet] La banca dati statistica delle professioni Inail: uno strumento per conoscere, monitorare e ridurre i rischi dei lavoratori. (2018) [cited 2018 May 29]. Available from: https://www.istat.it/it/files/2016/06/03_Brusco.pptx;
- Istituto Nazionale Assicurazione Infortuni sul Lavoro (INAIL) [Internet]. Malattie professionali: ultimi dati del 2015. (2016) [cited 2018 May 29]. Available from: https://www.inail.it/cs/internet/docs/alg-dati-inail-2016-dicembre.pdf;
- D. Lgs. 9 aprile 2008, n. 81. Testo unico sulla salute e sicurezza sul lavoro. Gazzetta Ufficiale n. 101 del 30 aprile 2008 - Suppl. Ordinario n. 108;
- National Research Centre for Occupational Health and Safety Regulation (OHS) [Internet]. The Missing Link-Regulating Occupational Health and Safety Support. (2005) [cited 2018 May 29]. Available from: http://regnet.anu.edu.au/sites/default/files/publications/attachments/2015-05/WorkingPaper_35_0.pdf;
- Trout DB. General Principles of Medical Surveillance: Implications for Workers Potentially Exposed to Nanomaterials. Journal of Occupational and Environmental Medicine /American College of Occupational and Environmental Medicine. (2011) 53(6 0): S22-S24;
- Centers for Disease Control and Prevention (CDC) [Internet]. HIPAA Privacy Rule and Public Health. Guidance from CDC and the U.S. Department of Health and Human Services. (2003) [cited 2018 May 29]. Available from: https://www.cdc.gov/mmwr/preview/mmwrhtml/m2e411a1.htm;
- Koh D, Aw T-C. Surveillance in Occupational Health. Occup Environ Med (2003); 60:705–710;
- Tormoehlen LM, Tekulve KJ, Nañagas KA. Hydrocarbon Toxicity: A Review. Clin Toxicol (Phila). (2014) Jun;52(5):479-89;
- Mundt KA. Epidemiological Surveillance: A Management Tool for Occupational Health. J Ambul Care Manage. (1994) Apr;17(2):19-27;
- Istituto Superiore di Sanità (ISS) [Internet]. Questionario di valutazione degli stili di vita. [cited 2018 May 29]. Available from: http://old.iss.it/binary/ofad/cont/questionario%20giovani%20in%20forma.1225957648.pdf;
- GBD 2015 Risk Factors Collaborators. Global, Regional, and National Comparative Risk Assessment of 79 Behavioural, Environmental and Occupational, and Metabolic Risks or Clusters of Risks, 1990-2015: A Systematic Analysis for the Global Burden of Disease Study 2015. Lancet. (2016) Oct 8;388(10053):1659-1724;
- Centro Nazionale di Epidemiologia, Sorveglianza e Promozione della Salute (Epicentro) [Internet]. La Sorveglianza Passi. Sovrappeso e obesità. (2017) [cited 2018 May 29]. Available from: http://www.epicentro.iss.it/passi/dati/sovrappeso.asp;
- Centro Nazionale di Epidemiologia, Sorveglianza e Promozione della Salute (Epicentro) [Internet]. La Sorveglianza Passi. Attività fisica. (2017) [cited 2018 May 29]. Available from: http://www.epicentro.iss.it/passi/dati/attivita.asp;
- Centro Nazionale di Epidemiologia, Sorveglianza e Promozione della Salute (Epicentro) [Internet]. La Sorveglianza Passi. Consumo di alcol. (2017) [cited 2018 May 29]. Available from: http://www.epicentro.iss.it/passi/dati/alcol.asp;
- Centro Nazionale di Epidemiologia, Sorveglianza e Promozione della Salute (Epicentro) [Internet]. La Sorveglianza Passi. Abitudine al fumo. (2017) [cited 2018 May 29]. Available from: http://www.epicentro.iss.it/passi/dati/fumo.asp.ight pie).