Frailty in Emergency Departments: a new challenge? A risk factor and an unsolved health demand marker
Laura Morciano,1 Gennaro Cerone,1 Cristina Ambrosone,1 Emanuele Caredda,1 Francesca Di Gaspare,1 Francesca Lucaroni,1 Stefania Moramarco,1 Stefano Orlando,1 Jacopo Maria Legramante,2 Alessia Pesaresi1
1 Department of Biomedicine and Prevention, University of Rome Tor Vergata, Rome, Italy
2 Department of System Medicine, University of Rome Tor Vergata, Rome, Italy
Introduction
The ageing transformation of western societies is deeply challenging for health systems and their organisation.1 Demographic changes, resulting in an ageing population, are often reported as some of the main drivers of the growth in health spending.2 This is partly true, but does not consider some emerging conditions caused by demographic transition.3 In fact, an ageing population requires some accuracies that are not met in western hospital organisation. Frailty represents the most significant emerging issue related to elderly people, and is a new approach to the entire spectrum of problems associated with these patients. Recently, Gilardi et al.4 highlighted frailty as a powerful predictor for the use of services and health demand. The emergency department (ED) is included in this phenomenon, as the authors indirectly described in investigating the main characteristics of the population accessing the ED.5 In fact, the ED represents the first point of contact with the health system, especially when continuum of care is not well established and health needs remain unmet.6
Many authors have reported5,7,8 the complex interactions between health systems and frailty, focusing on inappropriate response and inadequate services offered. It is clear that frailty should be considered as a complex of social, economic, mental and physical conditions (including ADL and IADL, housing and social networks), requiring a proper continuum of care to avoid the explosion of health demand.9 In our previous work, we acknowledged that elderly people are responsible for the 45% of ED visits and represent the 87% of frequent users.5 The aspects of frailty directly associated with this demand remained unclear. It is also important to assess whether health conditions are the only drivers of ED use. We hypothesise that other frailty problems and conditions can modulate and distort this phenomenon. Anecdotal reports refer to ED access directly linked to poverty situations, for instance.
Finally, if this hypothesis is confirmed, health systems will require a renewed continuum of care specifically devoted to solving the problems associated with frailty. We still need to know the ‘ingredients’ of frailty directly involved in this increasing demand: housing, social problems, economic and poverty problems, but also a new approach to considering health problems from the perspective of frailty. Frailty is not an illness per se but a condition that can weaken or impair general health status and generate health problems.10
The aim of the study is to evaluate the prevalence of frailty in the ED setting, using a multidimensional questionnaire. Moreover, we also would like to estimate the incidence of adverse outcomes and their correlation with frailty in the same population.
Materials and Methods
Study Design
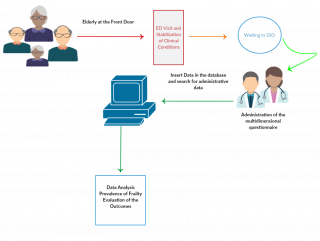
The study was designed as an integrated model in which data collected with a cross-sectional survey were linked with administrative database to follow patients and evaluate outcomes during the follow up period. During the calendar year 2017, a randomised sample of elderly (≥ 65 years old) inpatients attending the ED, was tested to estimate the presence and prevalence of frailty. After their stabilisation, patients attended in the Short-Stay Observation (Unit/Ward) were recruited and, after the signature of informed consent, medical students, under the supervision of a qualified psychologist, administered the multidimensional questionnaire. Following the completion of the cross-sectional survey, through access to administrative database, investigators collected data connected both with the access to the ED referred to the interview, and the subsequent accesses made during the follow-up period. The censor date was fixing at 31st December 2018. Figure 1 shows the flows of the study. The results of the questionnaires and the administrative information were collected in a database and analysed using the software SPSS Statistics (Illinois, v. 23).
Figure 1. Diagram flows of the study.
Sample Size
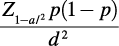
Giving the principal goal of the study, the sample size population was calculated according to the following formula for cross-sectional surveys:11
We considered a confidence limit (CL) of 95% and a precision of 5% with an estimated prevalence rate of frailty of 20%. In agreement with these parameters, the sample size needed was 196 subjects.
Randomisation
The randomisation process was performed over 6 months according to a simple sampling technique. The recruitment started on a random day and continued on a clockwise and weekly basis. The frequency of interview per days was proportional to monthly patient admissions to the ED.
Inclusion and exclusion criteria
The only inclusion criterion was represented by patients’ age of 65 or more. No exclusion criteria were applied.
Materials
To assess frailty, the authors adopted a multidimensional evaluation instrument, the Geriatric Functional Evaluation (GFE), a revised version of the Geriatric Functional Rating Scale, designed, tested, and validated by Grauer and Birnbom (1975) and introduced in Italy by the working group of the Epidemiology of the University of Rome Tor Vergata.12 The questionnaire provides a score between -108 and +90 and describes 4 areas of impairment (physical, mental, social and economic) establishing four classes of risk: robust, pre-frail, frail and very frail.
The administrative database of the Hospital has provided the following variables, both for the access linked to the interview day, and for the followings:
- Identification code for each patient;
- Birth date;
- Age;
- Gender;
- Civil state;
- Graduation;
- Number of accesses in the follow-up period;
- Symptoms at the front door;
- Triage code;
- Diagnosis of the ED;
- Closing date of the ED;
- Outcome of the visit.
Frequent users were identified as patients with four or more accesses per year.
Results
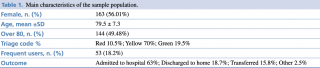
Given the possibility of a certain number of dismisses, the authors decided to interview a higher number of patients to assess the main aim of the study. According to this, the study population consisted of 291 patients, 163 women and 128 men, with a mean age of 79.5 ± 7.3 years. Table 1 shows the main characteristics of the participants.
Table 1. Main characteristics of the sample population.
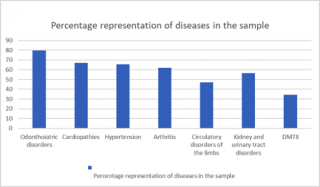
The average time spent in emergency department was 3.3 days (SD ± 2.1), with a maximum of ten days. Only nine patients (3.1%) were discharged within 24 hours. Frequent users corresponded to the 18.2% of the population, and four patients recorded more than ten admissions. Patients had numerous comorbidities, and about 30% of them declared more than 10 diseases. The mean number of diseases was 8 ± 2.6, with a maximum of 16 comorbidities. As shown in the Figure 2, odonthoiatric disorders represented the most common pathology in the sample (79.6%), followed by cardiopathies (67%), arterial hypertension (187, 65.6%), arthritis (179, 61.9%), circulatory disorders of the limbs (134, 47%), diseases of the kidneys and urinary tract (163, 56.4%). A significant percentage of the population was suffering from type II diabetes (98, 34.4%), while suffered from anaemia n?? (23.5%) and 58 (20%) were cancer patients. Other significant clinical conditions, reported by interview, were the use of dental prostheses (94.8%) and glasses (71.2%).
Figure 2. Diseases representation.
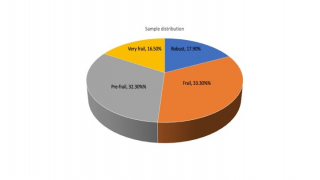
Frailty was present in the 33.3% of the patients, with 16.5% being severely frail and 32.3% pre-frail. Among participants, only 17.9% appeared robust (Figure 3).
Figure 3. Frailty distribution.
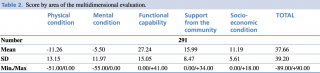
Frailty analysed with the multidimensional evaluation shows a widespread condition, in which physical decay is only one of the many factors involved in determining frailty itself. Table 2 shows the scores for the questionnaire’s areas (physical condition, mental condition, functional capabilities, support from the community, socio-economic condition).
Table 2. Score by area of the multidimensional evaluation.
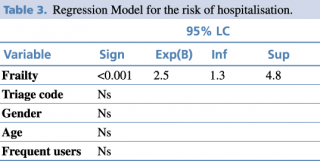
Older patients, aged 80 or more, have a higher risk of being frail (OR 3.1, LC 1.9-4.9; p<0.05), as well as the female ones (OR 2.05, LC 1.3-3.3; p<0.001). Frail patients have a higher risk of being hospitalised respect to the non-frail elderly (RR 2.5, LC 1.3-4.7; p<0.05). Among frail patients, those alone have a higher risk of hospitalisation (RR 2.9, LC 1.1-4.6; p<0.05). No statistically significant differences were observed between frail and non-frail patients with respect to the urgency code or number of accesses in ED. To identify the main causes of hospitalisation, a logistic regression model was constructed, as shown in the table 3, in which the only outcome that predict hospitalisation is represented by frailty (RR 2.5, LC 1.3-4.8; p<0.001), regardless of the urgency code, age, and other possible variables included in the model.
Table 3. Regression Model for the risk of hospitalisation.
Discussion
The results of this study highlight the importance of screening frailty in the ED3-5, to predict the impact on future worst outcomes related to ED’s accesses and effectively transmit this information to other care services and assistance settings. Frailty represents an important challenge for Public Health, and it needs an effective preventive approach in all settings to avoid inappropriate responses. In fact, the prevalence of frailty found in this study, more than 50% of patients frail or severely frail, is much higher than that reported in the community settings.13 The instrument used and the choice of setting, which allowed the authors to study frailty with a multi-dimensional evaluation, that is uncommon for the ED setting,14-17 could explain this result. Actually, despite many studies investigated frailty in the ED, more often the frailty screening tools were based on clinical conditions.18 Another key issue is the statistically significant correlation between frailty, loneliness and ED use. Frail elderly are more often alone than non-frail older adults, pointing the requirement of alternative support to take care of them. The high number of hospitalisations after ED visiting by frail patients, as confirmed by the regression model, suggests that, irrespective of underlying clinical conditions, an unsolved assistance demand represents the main factors for requiring ED access.9,19 This unanswered question leads frail older adults to turn to the only place where they can express their need for care. Therefore, hospitalisation of frail elderly represents the failure of continuum of care, highlighting the lack of territorial care, both health and social. Moreover, the high level of comorbidities makes hard the management of these patients in an emergency setting,20 and expose them to negative consequences. Furthermore, despite in this study the association between frailty and frequent use of ED or urgency code is no statistically significant, the available data suggests that frailty substantially affects the use of health settings and contributes to the worst outcomes.21 As a recent study confirms,5 elderly patients itself have a significant higher risk in accessing ED with an urgency triage code (OR 2.5; LC 1.06-5.7) and becoming frequent users (OR 2.2; LC 1.04-4.8) and because of these, they remain in the ED for a long time, waiting for hospitalisation and contributing to overcrowding. Considering frail patients in the ED, these individuals have worse outcomes in all the fields considered: triage code, accesses per year, hospitalisation, institutionalisation and death. The lack of evidence in these fields in our study could depends by the little number of “robust” elderly that we found and the impossibility to know the outcomes occurred out of the ED. Indeed, only 17.9% of the elderly patients who accessed the ED were considered ‘robust’, while the rest of the sample was frail or pre-frail.
This study has some limitations. Firstly, it was not possible to monitor patients after their discharge from the ED in order to assess some later outcomes, such as mortality or institutionalisation. Secondly, we do not know whether frequent ED users and other patients visited different hospitals.
Conclusion
Frailty is clearly a complex condition, combining social, emotional, physical, mental and economic variables in a unique syndrome. When its various components are not recognised and controlled, it leads to a sudden decline and frequent visits to the ED, worse triage codes, and more frequent hospitalisation. We consider our results a marker of a poor and insufficient continuum of care.
The Emergency Department still represents the main point of access to health systems for many patients.6 Too many times, it must cope with poor health and social services. More often, frail elderly patients require an integrated approach, which combines both social and health care.22 As this study confirms, if patients’ social needs are ignored, health status will worsen until the individual concerned is forced to seek medical attention in the ED. This unsolved demand produces an overflow of patients in the ED, resulting in an increase in waiting lists and hospitalisations, and a whole range of negative consequences for the population and for the health system.
One of the most important unsolved demand concerns loneliness: social transformation increasingly means that elderly people became alone and in some cases not self-sufficient.23 The study shows that this is one of the main reasons why elderly patients are admitted to the ED.
This phenomenon is significantly reduced when elderly people find a form of social support, even as an alternative to the family unit.24 It can be argued that we are in fact dealing with a question that must be decoded in terms of its social and health significance.
Considering the phenomenon from an economic and sustainability point of view, it is easy to understand that it would be much more beneficial to provide frail subjects with both health and social support in their homes rather than in hospitals, for as long as possible.25
In conclusion, it is fundamental to consider that hospitalised frail elderly patients incur risks to their own physical (hospital infections, pressure sores, loss of function: incontinence, etc.) and mental health (confusion, loss of memory, delirium, etc.), that requires special attention when patients just arrived in ED. Early detection of frailty status, considering in its multidimensional aspect, can improve both the management and clinical outcomes for these patients.
References
- Mate KS, Berman A, Laderman M, Kabcenell A, Fulmer T. Creating Age-Friendly Health Systems - A Vision for Better Care of Older Adults. Healthc (Amst). 2018; 6(1): 4-6.
- Castles FG. The Future of the Welfare State: Crisis Myths and Crisis Realities. Int J Health Serv. 2002; 32(2): 255-77.
- Marć M, Bartosiewicz A, Burzyńska J, Chmiel Z, Januszewicz P. A Nursing Shortage - A Prospect of Global and Local Policies. Int Nurs Rev. 2018.
- Gilardi F, Scarcella P, Proietti MG, Capobianco G, Rocco G, Capanna A, Mancinelli S, Marazzi MC, Palombi L, Liotta G. Frailty as a Predictor of Mortality and Hospital Services Use in Older Adults: A Cluster Analysis in a Cohort Study. Eur J Public Health. 2018; 28(5): 842-6.
- Legramante JM, Morciano L, Lucaroni F, Gilardi F, Caredda E, Pesaresi A, Coscia M, Orlando S, Brandi A, Giovagnoli G, Di Lecce VN, Visconti G, Palombi L. Frequent Use of Emergency Departments by the Elderly Population When Continuing Care Is Not Well Established. PLoS One. 2016; 11(12): e0165939.
- Dermody G, Sawyer P, Kennedy R, Williams C, Brown CJ. ED Utilization and Self-Reported Symptoms in Community-Dwelling Older Adults. J Emerg Nurs. 2017;4 3(1): 57-69.
- Mantelli S, Jungo KT, Rozsnyai Z, Reeve E, Luymes CH, Poortvliet RKE, Chiolero A, Rodondi N, Gussekloo J, Streit S. How General Practitioners Would Deprescribe in Frail Oldest-Old with Polypharmacy - The LESS Study. BMC Fam Pract. 2018; 19(1): 169.
- Saum KU, Schöttker B, Meid AD, Holleczek B, Haefeli WE, Hauer K, Brenner H. Is Polypharmacy Associated with Frailty in Older People? Results from the ESTHER Cohort Study. J Am Geriatr Soc. 2017; 65(2): e27-e32.
- Windhaber T, Koula ML, Ntzani E, Velivasi A, Rizos E, Doumas MT, Pappas EE, Onder G, Vetrano DL, Roudriguez Laso A, Roudriguez Manjas L, Illario M, Roller-Wirnsberger RE; ADVANTAGE JA WP8 group. Educational Strategies to Train Health Care Professionals Across the Education Continuum on the Process of Frailty Prevention and Frailty Management: A Systematic Review. Aging Clin Exp Res. 2018; 30(12): 1409-15.
- Boers M, Cruz Jentoft AJ. A New Concept of Health Can Improve the Definition of Frailty. Calcif Tissue Int. 2015; 97(5): 429-31.
- Charan J, Biswas T. How to Calculate Sample Size for Different Study Designs in Medical Research? Indian J Psychol Med. 2013; 35(2): 121-6.
- Scarcella P, Liotta G, Marazzi MC, Carbini R, Palombi L. Analysis of Survival in a Sample of Elderly Patients from Ragusa, Italy on the Basis of a Primary Care Level Multidimensional Evaluation. Arch Gerontol Geriatr. 2005; 40(2): 147-56.
- Collard RM, Boter H, Schoevers RA, Oude Voshaar RC. Prevalence of Frailty in Community-Dwelling Older Persons: A Systematic Review. J Am Geriatr Soc. 2012; 60(8): 1487-92.
- Pilotto A, Ferrucci L, Franceschi M, D'Ambrosio LP, Scarcelli C, Cascavilla L, Paris F, Placentino G, Seripa D, Dallapiccola B, Leandro G. Development and Validation of a Multidimensional Prognostic Index for One-Year Mortality from Comprehensive Geriatric Assessment in Hospitalized Older Patients. Rejuvenation Res. 2008; 11(1):151-61.
- Meldon SW, Mion LC, Palmer RM, Drew BL, Connor JT, Lewicki LJ, Bass DM, Emerman CL. A Brief Risk-Stratification Tool to Predict Repeat Emergency Department Visits and Hospitalisations in Older Patients Discharged from Thevemergency Department. Acad Emerg Med. 2003; 10(3): 224-32.
- Peters LL, Boter H, Buskens E, Slaets JP. Measurement Properties of the Groningen Frailty Indicator in Home-Dwelling and Institutionalized Elderly People. J Am Med Dir Assoc. 2012; 13(6): 546-51.
- Chiovenda P, Vincentelli GM, Alegiani F. Cognitive Impairment in Elderly ED Patients: Need for Multidimensional Assessment for Better Management after Discharge. Am J Emerg Med. 2002; 20(4): 332-5.
- Theou O, Campbell S, Malone ML, Rockwook K. Older Adults in the Emergency Department with Frailty. Clin Ger Med. 2018; 34: 369-86
- Tsai MH, Xirasagar S, Carroll S, et al. Reducing High-Users’ Visits to the Emergency Department by a Primary Care Intervention for the Uninsured: A Retrospective Study. Inquiry. 2018; 55: 46958018763917.
- Craswell A, Marsden E, Taylor A. Wallis M. Emergency Department Presentation of Frail Older People and Interventions for Management: Geriatric Emergency Department Intervention Saf Health 2016 2: 14.
- Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in Elderly People. Lancet. 2013; 381(9868): 752-62.
- Kodner DL. Whole-System Approaches to Health and Social Care Partnerships for the Frail Elderly: An Exploration of North American Models and Lessons. Health Soc Care Community. 2006; 14(5): 384-90.
- Wenger GC, Burholt V. Changes in Levels of Social Isolation and Loneliness among Older People in a Rural Area: A Twenty-Year Longitudinal Study. Can J Aging. 2004; 23(2): 115-27.
- Thompson EH Jr, Futterman AM, Gallagher-Thompson D, Rose JM, Lovett SB. Social Support and Caregiving Burden in Family Caregivers of Frail Elders. J Gerontol. 1993; 48(5): S 245-54.
- Featherstone A. Developing a Holistic, Multidisciplinary Community Service for Frail Older People. Nurs Older People. 2018; 30(7): 34-40.