Physical frailty and barriers to health care access among older adults in urban and rural areas/Kurdistan region of Iraq
Sivar A. Qadir,1 Stefania Moramarco,2 Shahla O. Salih,3 Faiq B. Basa,4 Leonardo Emberti Gialloreti2
1 Directorate of Health, Sulaymaniyah, Kurdistan Region, Iraq
2 Department of Biomedicine and Prevention, University of Rome Tor Vergata, Rome, Italy
3 Department of Statistics and Informatics, University of Sulaymaniyah, Iraq
4 Rizgary Teaching Hospital, Erbil, Kurdistan Region, Iraq
Introduction
Frailty is characterized by a decrease in physiological reserves and a raised liability to possible stressors, a series of age-related deficiencies. Therefore, leading to a loss of resistance to acute physical, psychological and socioeconomic stressors, and even a diminished ability to function normally, placing the individual at a steadily increasing risk of negative consequences, such as hospitalizations and delirium.1-3 Ferrucci and Fried were the first to identify frailty as a hallmark of accelerated aging, and it is now viewed as a severe outcome of the aging process.4
The world's population is aging more and more quickly: the percentage of older adults will climb from 11% to an estimated 22% by 2050, bringing the total of older adults’ population to two billion.5
Growing scientific attention is being paid to frailty all over the world, particularly in countries with growing older adult populations.6,7 Health care providers are focusing more on recognizing and responding to the factors that influence older persons at risk of rapid declines in health and functionality. No agreement has been reached however in terms of operational parameters and epidemiological studies employed in several settings. The result is an increased risk of negative health consequences, hospitalization, and greater mortality.8
The first thing to do is recognize and comprehend the medical assistance that older persons require, taking into consideration the contexts in which they communicate and function, to fulfil their health requirements. In order to achieve this, specialized geriatric evaluation tools are required to detect frail older persons and address their needs. The first step toward successfully implementing public health interventions and prevention measures is to identify older adults who are weak or are on the verge of becoming so.9 To calculate the frailty index, a comprehensive geriatric assessment is required.10
According to Iraq’s Ministry of Health’s annual statistical report, the percentage of the older adults’ population in Iraq climbed from 3.4% in 2010 to 5% in 2015, and will reach a predicted 7.2% in 2050.11,12 In Northern Iraq (the Kurdistan Region), the population was calculated at 5,122,747 in 2014, and 4% was 65 or older, a similar pattern can be seen.13
Nevertheless, health care for older persons in Iraq is poorly integrated into the health system due to a lack of Rehabilitation centres for older adults, a shortage of locally trained geriatric physicians or nurses, and a small number of practitioners who are not prepared to fully deal with such a rapid increase in the aging population.14 Because of the dearth of local geriatric postgraduate students, there are few geriatric physicians in the Kurdistan Region, according to our understanding of the local situation. There is a general shortage in the region’s healthcare system of geriatric programs, rehabilitation centres for older persons, and a system able to gather accurate information on prevalent health conditions among the older adults and respond to their needs.15 In terms of social connections, there are no specific designated areas for older persons to gather for social activities apart from traditional ones, including family visits, gathering in mosques or public café.16 Their social needs are unknown, due to a lack of comprehensive research about older adult citizens in the region.
Furthermore, few studies, offering sporadic data, have been undertaken in this context; the majority of them include older persons living in care homes, which are not representing the status of the majority of Iraq’s older adult population. According to a study conducted in Erbil in 2013, the majority of those living in nursing homes were aged between 61 and 80 (71.4%).17 The investigation in the rural area found that impairment increases with age, with a peak in mental and physical impairment (18.5%) for those aged 65 and over. Impairments are more common in low-income families than rich families, and less wealthy parents are much more likely to be found in rural areas than in metropolitan areas (41% vs. 36%).13
The main aim of this study was thus to investigate a still unknown topic, i.e., physical frailty among older persons living in their homes in Northern Iraq (Kurdistan Region), to determine the barriers to healthcare services in the urban and rural areas (Directorate of Sulaymaniyah).
Methodology
Population and setting
This cross-sectional research was carried out from July 2020 to March 2021, through structured interviews. Involving a sample of (200) older persons (≥ 65 years old) living in their homes randomly selected in two different areas, one urban (Sulaymaniyah city-center) and one rural (Penjwen district), in the Kurdistan Region of Iraq were considered. Older adults living in nursing homes or hospitalized were not considered at this stage, as this was not the purpose of the research. Only Kurdish-speaking persons were interviewed, for ease of understanding. Participants were free to participate or not in the interview and answered independently or with the support of relatives. The study sample was collected from people’s homes. When direct face-to-face interviews were not possible – mainly due to the Covid-19 pandemic,18 phone contact was made, obtaining the relative contact details from friends and health centres. Those who refuse to participate or only answered half of the questionnaire were removed from the total sample.
The Questionnaire
Two existing validated tools were used to create an ad hoc questionnaire:
- The short functional geriatric evaluation questionnaire (SFGE) was used to predict bad life outcomes among older persons. It has ten ordinal variables (age, gender, education, co-habitants, help if needed, involvement in social activities, receiving regular social assistance from NGOs, Government, or other people not living with the person, economic condition, energy and drive, health and functional status). A 34-point range, from -6 to +27 could be obtained, so that the person could be classified in one of the following four classes: robust (score ≤0), pre-frail (score 1-2), frail (score 3-9), and very frail (score ≥10).9 We made some alterations to the SFGE; for living arrangements, we added “living with children and other relatives”, and for receiving formal social assistance we altered to receiving formal social assistance from Government, NGO, or other people not living with them. For the financial situation we included the option “no work income/no State pension (score 0), “State pension (score -1)”, “still working (score 2)”. Regarding the economic condition if the older person could not get to the end of the month on their pension/pocket money or income, we identified as the main area for economic concern “buying food, medicine, and clothes and paying bills”, and “paying someone to do daily living or household tasks”. These alterations were made in order that the questionnaire becomes more suitable with the situation of the older adults in the region.
- The barriers to health care services questionnaire were used to investigate the challenges faced in accessing health care services. It contains nine assertions about obstacles to health care access for older adults who are likely to have a stroke (work responsibility, caring for others, regular doctors or none responsive to concern, fear of unneeded tests, serious illness or safety on street, transport and medical bills). Individuals could use a 3-point scale (no, moderately and very much) to respond.19
Questionnaires were translated into Kurdish language to facilitate understanding. Participants’ privacy was anonymized by assigning ID numbers to questionnaires like (Sulaymaniyah number 1, Penjwen Number 1, etc.), therefore not including identification data. The questionnaire data were later inserted and stored in Excel sheets.
The research was approved by the Ethics Committee of the College of Administration and Economics, Department of Statistics and Informatics, University of Sulaymaniyah (75/1 on 05.04.2021)
Statistical Analysis
The descriptive analysis included frequencies and percentages. Data were reported as an overall sample and then split between Sulaymaniyah and Penjewen. Data were analysed using the Statistical Package for Social Sciences (SPSS, version 22). The Pearson’s chi-square and Bonferroni correction tests were used to assess the differences between categorical variables. All p values were two-tailed, and p≤0.05 was considered statistically significant.
Results
The total sample included 200 older persons: 160 from Sulaymaniyah (80%), 40 from Penjwen (20%). The median age was 71 years, with 42.5% (85 persons) aged <70 years old, 39.0% (n. 78) aged 70-80 years old, 18.5% (n. 37) aged >80 years old, 52.0% (n. 104) were male. When considering the two areas separately (i.e., Sulaymaniyah vs. Penjwen), 52.5% (n. 84) of participants from the urban area were male vs. 50.0% (n. 20) in the rural area. The median age was 71 (43.1% aged <70, 39.4% aged 70-80, 17.5% aged >80 and 74.5 (40.0%) aged <70, 37.5% aged 70-80 and 22.5% aged >80 respectively).
In terms of education, 73% of the sample was illiterate (68.1% in Sulaymaniyah vs 92.5% in Penjwen), while only 4% (all from the urban area) had higher educational qualifications. Less than a quarter had attended elementary or secondary schools (26.9% vs. 7.5% respectively).
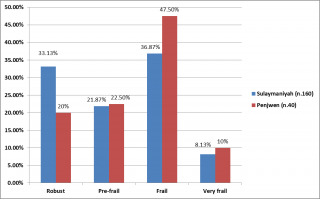
Table 1 presents some variables included in the SFGE, with results presented as a total then split by area of provenience. In the co-habitant item, 56.5% (n. 113) of older persons were living with a spouse (43.5% in Sulaymaniyah vs. 65% in Penjwen). Most of the older adult population received informal help when needed (83.1% vs. 72.5%) in the urban and rural areas respectively. Most of the older adult population (66.5%, n. 133) did not take part in any social activity (69.4% Sulaymaniyah vs. 55% Penjwen). Additionally, most of them (90.5%, n. 181) did not receive any formal social assistance from NGOs, Government, or other parties (90.6% Sulaymaniyah vs. 90% Penjwen).
Table 1: The SFGE evaluation questionnaire - Parameters: living conditions.
When considering financial support, nearly half of the sample (51.5%, 48.1% Sulaymaniyah vs. 65% Penjwen) did not have any work income or State pension, most were from the urban area. Half of the investigated population (49.50%, 79% Sulaymaniyah vs. 20% Penjwen) was concerned about not having enough income for their needs until the end of the month. This was reported to be due to most of the money being spent on necessities (97.5% Sulaymaniyah vs. 100% Penjwen), such as food, medicine, clothes, and bills. Only 2.5% (all from the urban area) could afford to pay somebody to help with household tasks.
Table 1: The SFGE evaluation questionnaire – Parameters.
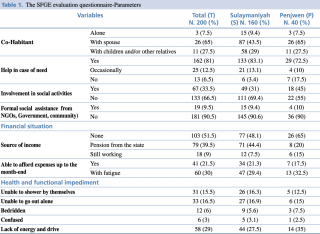
Regarding comparing data on the degree of frailty between Sulaymaniyah vs. Penjwen, the share of robust individuals was (20% in Penjwen vs. 31.13% in Sulaymaniyah), (22.5% in Penjwen vs. 21.87% in Sulaymaniyah) were in the pre-frail class, (47.50% in Penjwen vs. 36.87% in Sulaymaniyah) were in the frail class. The “very frail” class accounted for (8.13% of older persons in urban areas vs. 10% in rural areas).
Table 1. The SFGE evaluation questionnaire-Parameters.
Figure 1: Physical frailty score in Sulaymaniyah vs. Penjwen.
Regarding those who fall in the frail group, the total number of frail older adults in Sulaymaniyah and Penjwen were (78), (59 out of 160) in Sulaymaniyah and (19 out of 40) in Penjwen, the highest number of frail older persons were in the (70-80) age group in both regions, (27 out of 59) in Sulaymaniyah and (7 out of 19) in Penjwen with a very significant difference (p<0.01) between Sulaymaniyah and Penjwen (45.76% vs. 36.84%). In terms of gender, more females were placed in the very frail group, being higher in Sulaymaniyah vs. Penjwen (59.32% vs. 52.63%). Looking at the educational qualifications, less educated people were more at risk of frailty; among the illiterate, for example, Sulaymaniyah and Penjwen posted frailty scores of 82.05% and 100% p<0.01, respectively; values were significantly higher in the rural area.
Figure 1. Physical frailty score in Sulaymaniyah vs. Penjwen.
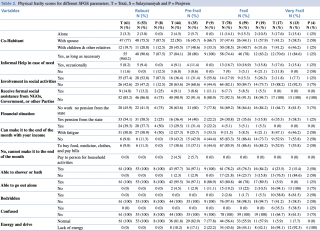
Table 2: Physical frailty scores for different social parameters.
The prevalence of physical frailty was investigated about some parameters documented in Table Ⅱ. Most of the older adults’ population (92.3%, n. 72) did not receive formal social assistance from NGOs, Government, or other people, posting frailty scores in Sulaymaniyah and Penjwen of 91.5% and 94.7%, p<0.01, respectively; scores were significantly higher in the rural area.
Looking at physical frailty scores by different income parameters, most of the older persons in our study did not have any work income or State pension. This factor increased the frailty score, with a significant difference between Sulaymaniyah vs. Penjwen (61.5% vs. 75%; p<0.01). Half of the investigated population was concerned about not having enough income to get by until the end of the month, since most of the money was spent on daily needs (i.e. food, medicine, clothes, bills), with a significant difference between the urban and rural areas (53.8% vs. 50%; p<0.01), thus, increasing the degree of frailty.
Looking at physical frailty scores by different health and functional parameters, most older adults’ participants still were able to shower by themselves, with a frailty score that was significantly different between urban and rural areas (76.3% vs. 84.2%; p<0.01). Additionally, most of them could go out alone, but the degree of frailty (22% vs. 10.5%) in Sulaymaniyah and Penjwen showed a highly significant difference (p<0.01). Most of the older persons were not bedridden, those that were bedridden totalled 1.7% vs. 5.3% in urban vs. rural areas, respectively, giving a very significant difference (p<0.01). Finally, most of the older adults’ population in our study had enough energy to perform normal daily tasks, but those lacking energy were placed in the “frail” class (44.1% in Sulaymaniyah vs. 42.1% in Penjwen, marking a highly significant difference (p<0.01).
Table 2: Physical frailty scores for different SFGE parameters.
Table 2. Physical frailty scores for different SFGE parameters. T = Total, S = Sulaymaniyah and P = Penjwen.
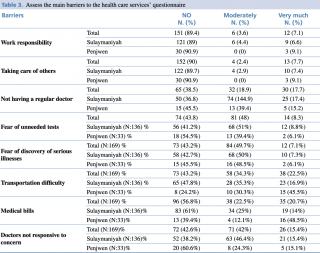
About barriers to health care services, out of the 200 participants in the two regions, 84.5% (n. 169) of the older adults’ population reported encountering obstacles to health care access. Regarding the availability of transportation services, 47.8% (n. 65) in Sulaymaniyah were satisfied and did not have transport difficulties, unlike older persons in Penjwen, who encountered transport difficulties (45.5%, n. 15 people), marking a highly significant difference (p<0.01). As regards medical bills, many older adults in Sulaymaniyah (61%, n. 83 people) did not encounter this problem, while in Penjwen half of the group (48.5%, n. 16 people) mentioned this difficulty, showing a highly significant difference (p<0.01).
Table 3: Assess the main barriers to the health care services’ questionnaire.
Table 3. Assess the main barriers to the health care services’ questionnaire.
Discussion
Concerns are growing as the world’s population ages, with every country seeing an increase in the number and proportion of older adult citizens.20 The number of persons aged 65 and over is expected to rise from 524 million in 2010 to nearly 1.5 billion in 2050, the majority of the growth coming in developing countries.21 As a result, all countries must ensure that their health and social systems are prepared to deal with the upcoming demographic shift. According to annual figures from the Ministry of Health in Iraq, the percentage of older persons aged 60 and over climbed from 3.4% in 2010 to 5% in 2015, and is expected to reach 7.2% in 2025.22 However, there is still a dearth of health data on older adults Iraqi citizens.23 We conducted a pilot study in Iraq’s Northern Region to evaluate the incidence of physical frailty and the barriers to access healthcare services in the country (Kurdish Region - Directorate of Sulaymaniyah). The effects of the setting on the situations of older individuals living in their homes were explored in both the urban and rural locations. This research was the first of its kind in this area. It appears that no previous studies have measured the frailty of older persons, even in urban areas of Kurdistan.
There was a statistically significant relationship between frailty and the 70-80 age group for the “very frail” score in urban vs. rural areas, particularly in the urban region, disagreeing with research data on Erbil24,25 and data from Jordan,26 which reported that frailty increased in the 65-70 age group. Unlike the results from this study, the previous study showed that the prevalence of frailty increased in persons over the age of 65 in a rural area of Turkey.27
There was a statistically significant relationship between frailty and female gender in Sulaymaniyah vs. Penjwen, particularly in the urban area, in agreement with findings from China, Japan, and southern Italy, reporting that frailest older persons were women,28,29 since on average women live longer than men, yet their health is worse.30
Illiterate individuals had the highest frailty scores, which rose in rural areas. Our findings regarding illiteracy and older adults’ frailty are corroborated by the study which concluded that the majority of frail older persons did not receive any formal education (52%).24 Additionally, our data concerning frailty among rural older persons tallied with previous data reported in the rural area of Turkey. The percentage of participants with less than three years of schooling was 84.3%, and it was seen that less-educated older persons were more vulnerable to the risk of frailty.27
In most cases, intergenerational support flowed in both directions.31 Families, particularly adult children, were the primary source of support and care for their older adults’ relatives, but older persons themselves frequently cared for their relatives.31 In our study we found that the majority of older persons were living with a spouse in Sulaymaniyah and Penjwen, the numbers were higher in the urban area. Moreover, most of them received informal help when they needed support, with a large number of participants never having received any formal social assistance, either in the urban or in the rural area. This finding is in line with the results of a previous study,32 according to study, physically challenged older persons are more prone to feelings of loneliness and isolation, which can lead to health problems, diminished functioning, and mental health complications, including depression.33
A large number of older persons in our study did not have any work income or public pension in both areas, with frailty scores being higher in the rural area. Half of the study population in Sulaymaniyah and Penjwen, especially in the urban area, were concerned about not having enough income to get by until the end of the month, because most of the money was spent on necessities and paying bills, with frailty scores being higher in Sulaymaniyah. The situation becomes worse when older adults need medications for chronic diseases, as reported by Faiq et al., who revealed that 75.5% of Kurdish older adults needed extra money to care for their health.34 The lack of a health information system that might routinely collect information on older adults and identify relative needs has a significant impact on increasing frailty among the older persons in Region.35
According to our findings, rising frailty in Penjwen is associated with a lack of healthcare for rural residents. One probable explanation is that urban communities have better access to physical activity than rural communities.36 Rural older people’s poor health is directly related to their low socioeconomic level, with a higher poverty rate and poorer health, meaning they have a greater need for services and resources than older people in urban regions.37
The results of our study showed that more than a quarter of the older persons in the Penjwen area do not have regular access to doctors’ care, which plays an important role in increasing frailty. As a result, access to healthcare services is a major concern, particularly for the rural population, since older adults have many more health problems and chronic diseases, necessitating more medical attention than the general population.38 Since only primary healthcare institutions exist in Kurdistan, persons residing in rural areas may only have access to junior doctors, who are not experts in the area of geriatrics. Furthermore, the quality of care is significantly inferior to that in urban regions due to a lack or scarcity of resources (such as doctors, medical personnel, laboratory testing, radiographic imaging, and drugs). Patients must travel a considerable distance to reach better healthcare facilities in Kurdistan’s tertiary centres, which are only located in the country’s largest cities if their health needs are not met where they live.39 As a consequence, integrating the urban and rural healthcare systems is a crucial step towards narrowing the gap in health care access between the two locations.40
Almost half of the population in the Penjwen area had great transport difficulties, with a highly significant difference compared with the other region. A previous study demonstrated a relationship between frailty, healthcare constraints, and transportation, and is considered to be one of the most serious concerns for the growing older adults’ population in rural areas.41,42 Since personal satisfaction is a crucial component of wellbeing for the older adults’ population, there is a link between a lack of mobility and a low level of life satisfaction, isolation, loneliness, and self-reported bad health, especially in rural areas.43
Additionally, older persons in the rural area came up against the barrier of medical bills to a high degree, with a highly significant difference compared with the urban area. Since out-of-pocket payments are the major source of financial stress for rural residents, cost concerns among older adults are mostly linked to supplemental insurance coverage. Cost, accessibility, lack of information, and caring for others are all obstacles to receiving healthcare, according to other studies.44
Study limitations:
- Due to the lockdown and COVID-19 pandemic only 200 samples of older adults were taken.
- Some older adults refused to participate and some of them just answered half of the questionnaire, so those samples were deleted from the total sample.
- Lack or insufficient knowledge and research on the older adult’s situation in Kurdistan region of Iraq and lack of an electronic health information system that can monitor situation of elderly continuously.
Possible public health implications:
This study can raise awareness of the health authorities on the situation of older adults regarding their social, financial and physical conditions and the differences between the rural and urban regions, including the differences in the barriers to health care services that are faced by older adult in both locations, so that the policy makers can provide electronic health information system that continuously monitor health of the older adults in all regions and provide geriatric intervention programs accordingly, such as training medical staffs on geriatric services and providing geriatric home care services, improving their financial situation by providing insurance for the older adults, improving their physical situation by increasing rehabilitation centres and providing specific places for social activities of older adults in order that they remain active in both rural and urban region especially in the rural regions.
Conclusion and recommendation
Physical fragility is severe among older people and given the reversible evolution of the frailty phenotype from pre-frailty to frailty, older people, particularly women, face a variety of health challenges. In comparison to metropolitan areas, restrictions on older people’s healthcare access have increased in rural areas. The older adult population in Kurdistan is victims of a non-responsive medical system due to a shortage of older adults Rehabilitation Centres and local geriatricians or physicians trained in geriatrics. Older people in Iraq are struggling to cope with everyday living, exacerbated by the country’s ongoing violence and instability, which has harmed the older adults’ health and emotional wellbeing.14 More efforts are being made to promote services for older persons, notably in the area of the environment, social activities, entertainment, security, and transportation.
Funding: The research was not granted any specific fund
Conflict of interest: The researcher claims no conflict of interest to declare
References
- De Vries N, Staal J, Van Ravensberg C, Hobbelen J, Rikkert MO, Nijhuis-Van der Sanden M. Outcome Instruments to Measure Frailty: A Systematic Review. Ageing Research Reviews. 2011;10(1):104-14.
- Kojima G, Iliffe S, Walters K. Frailty Index as a Predictor of Mortality: A Systematic Review and Meta-Analysis. Age and Ageing. 2018;47(2):193-200.
- Jung H-W. Frailty as a Clinically Relevant Measure of Human Aging. Annals of Geriatric Medicine and Research. 2021;25(3):139.
- Sekhon H, Minhas S. A Study of Activities of Daily Living of Elderly in an Urban Community of North India. Sch J App Med Sci. 2014;2(4):1450-4.
- Sander M, Oxlund B, Jespersen A, Krasnik A, Mortensen EL, Westendorp RGJ, et al. The Challenges of Human Population Ageing. Age and Ageing. 2015;44(2):185-7.
- Tkatch R, Musich S, MacLeod S, Alsgaard K, Hawkins K, Yeh CS. Population Health Management for Older Adults: Review of Interventions for Promoting Successful Aging across the Health Continuum. Gerontology and Geriatric Medicine. 2016;2:2333721416667877.
- Hu S, Tang S, Liu Y, Zhao Y, Escobar M-L, De Ferranti D. Reform of How Health Care Is Paid for in China: Challenges and Opportunities. The Lancet. 2008;372(9652):1846-53.
- Bouillon K, Kivimaki M, Hamer M, Sabia S, Fransson EI, Singh-Manoux A, et al. Measures of Frailty in Population-Based Studies: An Overview. BMC Geriatrics. 2013;13(1):1-11.
- Capanna A, Scarcella P, Gilardi F, Mancinelli S, Palombi L, Marazzi MC, et al. Sensitivity and Specificity of a Short Questionnaire to Screen Frailty in the Community-Dwelling Older Population. Advances in Aging Research. 2018;07(03):52-63.
- Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in Elderly People. The Lancet. 2013;381(9868):752-62.
- Desa U. United Nations Department of Economic and Social Affairs, Population Division. World Population Prospects: The 2015 Revision, Key Findings and Advance Tables. Online Edition UN DESA, New York. 2015.
- Ibrahim AA, Ai-Lami F, Al-Rudainy R, Khader YS. Mental Disorders among Elderly People in Baghdad, Iraq, 2017. Inquiry. 2019;56:46958019845960.
- Sindi A, Balakrishnan R, White G. Demographic Survey: Kurdistan Region of Iraq. United Nations International Organisation for Migration; 2018.
- Hussain HY. Elderly, Health and Socio-Demographic Profile in Iraq, the Context of Conflict, Violence and Social Exclusion, Systematic Review. Middle East Journal of Age and Ageing. 2016;83(4013):1-8.
- Emberti Gialloreti L, Basa FB, Moramarco S, Salih AO, Alsilefanee HH, Qadir SA, et al. Supporting Iraqi Kurdistan Health Authorities in Post-conflict Recovery: The Development of a Health Monitoring System. Front Public Health. 2020;8:7.
- Othman N. Situation of Older People in Kurdistan 2005.
- Ali S, Alhagbaker J, Shabila N. Daily Living Activities among Geriatric Residents at Geriatric Homes in Erbil and Sulaimaniyah Cities, Kurdistan Region. Zanco Journal of Medical Sciences. 2017;21(1):1619-28.
- Tadesse S, Muluye W. The Impact of COVID-19 Pandemic on Education System in Developing Countries: A Review. Open Journal of Social Sciences. 2020;08(10):159-70.
- Fitzpatrick AL, Powe NR, Cooper LS, Ives DG, Robbins JA. Barriers to Health Care Access among the Elderly and Who Perceives Them. American Journal of Public Health. 2004;94(10):1788-94.
- Shrestha LB. Population Aging in Developing Countries: The Elderly Populations of Developing Countries Are Now Growing More Rapidly Than Those in Industrialized Nations, Thanks to Health Advances and Declining Fertility Rates. Health Affairs. 2000;19(3):204-12.
- Nations U. World Population Prospects: The 2015 Revision. United Nations Econ Soc Aff. 2015;33(2):1-66.
- Ibrahim AA, Ai-Lami F, Al-Rudainy R, Khader YS. Mental Disorders among Elderly People in Baghdad, Iraq, 2017. INQUIRY: The Journal of Health Care Organisation, Provision, and Financing. 2019;56:0046958019845960.
- Tariq E, Lafta R. A Profile on Health-Care Services for Old in Baghdad. Mustansiriya Medical Journal. 2018;17(1):52.
- Sangar M, Karem F, Alireza N, Muaf A. Old Age Satisfaction Regarding Geriatric Home Services in Erbil City. Journal of Medicine and Life. 2015;8(Spec Iss 3):195.
- Ali SS, Alhagbaker JM, Shabila NP. Daily Living Activities among Geriatric Residents at Geriatric Homes in Erbil and Sulaimaniyah Cities, Kurdistan Region. Zanco Journal of Medical Sciences (Zanco J Med Sci). 2017;21(1):1619-28.
- Naylor M. Delirium, Depression Often Overlooked. American Journal of Nursing. 2003;103(5):116-.
- Çakmur H. Frailty among Elderly Adults in a Rural Area of Turkey. Medical Science Monitor: International Medical Journal of Experimental and Clinical Research. 2015;21:1232.
- Liu W, Puts M, Jiang F, Zhou C, Tang S, Chen S. Physical Frailty and Its Associated Factors among Elderly Nursing Home Residents in China. BMC Geriatrics. 2020;20(1):1-9.
- Shibasaki K, Kin SK, Yamada S, Akishita M, Ogawa S. Sex-Related Differences in the Association between Frailty and Dietary Consumption in Japanese Older People: A Cross-Sectional Study. BMC Geriatrics. 2019;19(1):1-9.
- Corbi G, Cacciatore F, Komici K, Rengo G, Vitale DF, Furgi G, et al. Inter-Relationships between Gender, Frailty and 10-Year Survival in Older Italian Adults: An Observational Longitudinal Study. Scientific Reports. 2019;9(1):1-7.
- Kowal P, Williams S, Jiang Y, Fan W, Arokiasamy P, Chatterji S. Aging, Health, and Chronic Conditions in China and India: Results from the Multinational Study on Global Ageing and Adult Health (SAGE). Aging in Asia: Findings from New and Emerging Data Initiatives: National Academies Press (US); 2012.
- Schröder-Butterfill E. Inter-Generational Family Support Provided by Older People in Indonesia. Ageing & Society. 2004;24(4):497-530.
- Dirik A, Cavlak U, Akdag B. Identifying the Relationship among Mental Status, Functional Independence and Mobility Level in Turkish Institutionalized Elderly: Gender Differences. Archives of Gerontology and Geriatrics. 2006;42(3):339-50.
- Faiq SF, Faraj SA, Amin A, Robinow A, Loftus S, Shawis T. Depression in the Older People: A Perspective from Kurdistan of Iraq. Middle East Journal of Age and Ageing. 2017;14(3).
- Moramarco S, Basa FB, Alsilefanee HH, Qadir SA, Gialloreti LE. Developing a Public Health Monitoring System in a War-Torn Region: A Field Report from Iraqi Kurdistan. Disaster Medicine and Public Health Preparedness. 2020;14(5):620-2.
- Kinsella K, Velkoff V. US Census Bureau. An Aging World. Washington DC. US Govt Printing Office. series P95/01–1; 2001.
- Rogers CC. The Older Population in 21st Century Rural America. Rural America/ Rural Development Perspectives. 2002;17(2221-2019-2532):2-10.
- Dassah E, Aldersey H, McColl MA, Davison C. Factors Affecting Access to Primary Health Care Services for Persons with Disabilities in Rural Areas: A “Best-Fit” Framework Synthesis. Global Health Research and Policy. 2018;3(1):1-13.
- Quinn J. Letter from the Field: Health Security in Kurdistan. Journal of Human Security. 2011;7(2):47-53.
- World Health O, Organisation for Economic C-o, Development, International Bank for R, Development. Delivering Quality Health Services: A Global Imperative for Universal Health Coverage. Geneva: World Health Organisation; 2018.
- Glasgow N, Berry EH. Introduction to Rural Aging in Twenty-First Century America. Rural Aging in 21st Century America: Springer; 2013. p. 1-13.
- Herold M, Gordon T, Kaye K, Brockie E, Fuller T. Elderly and Disabled Rural Residents: A Continuing Transportation Issue. Rural Transportation Series. 2002(4).
- Glasgow N, Blakely RM. Older Nonmetropolitan Residents' Evaluations of Their Transportation Arrangements. Journal of Applied Gerontology. 2000;19(1):95-116.
- Ahmed SM, Lemkau JP, Nealeigh N, Mann B. Barriers to Healthcare Access in a Non‐Elderly Urban Poor American Population. Health & Social Care in the Community. 2001;9(6):445-53.